A Model for Living Well with Aging and Dementia
I want to share a presentation that I gave to a number of students in, a Legal Class for Aging at Forever Learning Institute. I have presented to a couple of classes and each time I think the presentation changed people’s minds about dementia and they had lots of significant questions. I have received great feedback and letters of appreciation each time.

I’d like to share this presentation with you as I did with them. Obviously, this information is coming from a first-person point of view on dementia, but more importantly, the model that I will share will provide a better understanding of what it means to live well when you have dementia.
The model is called “The Good Life Model”. I ran into it after I learned that I have dementia. I quickly realized there was little available from a person with dementia’s point of view.
In my search for information, I found a relatively obscure textbook by Laura Goldman and Nancy Howe. It was not cheap, even as a used textbook, but I guess that is the case with most college texts. The book is called “Better Living with Dementia”.
The book covers lots of different aspects of dementia. One chapter is about the “Lived Experience of Individuals with Dementia” the authors are trying to address a “first-person” point of view (POV) of a person with dementia.
It is at best; an academic’s understanding, but at least they tried. In their book there is a model called the “Good Life Model[1]” which was created in 1983 by Lawton. I first ran into this in a master’s Psych class at Western Michigan University.
This model can be applied to lots of things but, I like their application of the model to understand what affect things or changes have on a person with dementia.
I must mention though, if this model is applied inappropriately by a caregiver or clinician it can have a disastrous effect. I believe if misapplied it can be used quite manipulatively.
Let’s me explain. The problem most caregivers have with using this model is that they think they know what is best for the person in their care. Seems logical, right? No offense if you are Caregiver, but I have genuine concerns.
Here’s why, few people seldom look at the entire picture. The same applies to looking at what makes up a Good Life from a clinical POV.
For an example, in the book they sight an email of a poem written for a Care Giver at the beginning of this chapter. A Spouse writes the email / poem for her husband that cares for his mother.
“I am still a Person”
Written by a caregiver for her 70-year-old husband.
Things are at a slightly different stage. [my mom] has slowed down, with a little more confusion at times, more sleepiness, less balance, more use of the walker especially outside. She is still very sweet and has a smile and a nice word for everyone. Thank goodness for the Senior Center, where they talk about how remarkable [my mom] is, and how they all Love her. Rarely is she agitated, but it happens…
Can you see the issue?
- It is removed by two people
- Assuming her husband is 70 I’m guessing the women is at least 90 years old, the issues are normal for a 90-year-old women, and probably have nothing to do with dementia and more with aging.
- They put her in the Senior Center, but Mom does well there? Seems socialization was lacking in her environment and was improved by being with others and having activities.
- Last, the agitation might be more because her kids are not listening to her to her or spending time with her.
Personally, I see this as a splendid example of why caregivers and clinical people and academics get this wrong so often.
- They don’t listen
- They focus on solving the clinical problems first
- They focus on solving the family’s needs ahead of the persons
- They are quick to call AGING dementia
- They wait fair too long to help the person to make adjustments
So, let’s look at where the “Good Life Model” can be applied.
USING The Good Life Model
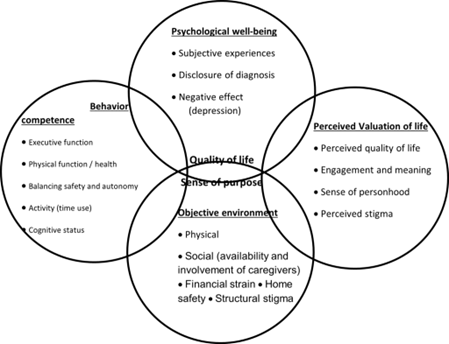
The top circle is Psychological Well-being and that would be North or 12 o’clock. The bottom circle is Objective Environment. The circle on the right or at 3 o’clock is the Perceived Value of Life, and to the West or at 9 o’clock is Behavioral Competence. In the center where the circles overlap, represents the Quality of Life and Sense of personhood. This sense of personhood is what makes us feel human. To be loved, and have a sense of wellbeing, have hope and all of that important stuff.
We all experience this, but we probably don’t think about it in these terms. We often talk about how people in their lives change, but we seldom put it in constructive terms.
So, let’s spend a few moments talking about each one of the aspects then talk about how they come together and how they can interact or balance with each other.
Psychological Well-being
Psychological well-being is a subjective experience, and positive experience effects, joy and happiness and negative emotions are obviously where sadness and even depression falls into this category.
This is where poor disclosure of a diagnosis comes about. If it is used improperly, or handled with insufficient information, it causes “internalization”. The same result would happen if you told someone they had some type of cancer and then told them nothing else.

What and how we learn about our diagnosis or how we come to accept it affects our physical and/or our mental health as well.
There are lots of examples for this, but I think you can understand the type of things that can push someone to the negative side.
Perceived Evaluation of Life
The circle to the right is about the quality of life. It’s about engagement in meaning and purpose. Obviously, engagement with others has suffered significantly during Covid. Socialization decreases depression because people that are isolated not only feel a lower sense of value of life, but it also affects phycological well-being and a sense of personhood.
Herein lies the rub. Because of the perceived stigmas associated with “Dementia” has such a bad connotation, that people treat you differently, because they don’t understand it. Worse, they say something like “you don’t look like you have dementia” or “you sound ok”. Hopefully, you can start to see perceived value of life is significantly diminished immediately upon hearing your diagnosis and not being given the right information about the disease.
Quality of Life – Sense of Personhood
If you look South, you will see items that are about the objective environment. That is the circle at 6 o’clock and it covers our physical location, physical well-being and those things which are physical.

Involvement of caregivers in this area seems to be a primary focus. It is things like how much focus we put on environment that can create a financial strain on the situation.
Far too often, money is at the root of many problems. On one call I heard a caregiver say… “My Mom wants to make sure we get the maximum inheritance so I don’t know how we can afford this.” My heart sunk. Forget inheritance, think about Mom. Yes, there is proper financial planning but…ouch.
Obviously, our environment and home safety plays into this. I know this is where the control part of Caregivers comes in. This is important! This differs though from what we perceived as avoiding a risk. This is where the real structural stigma of dementia does so much damage.
In other words, how people objectively act around people with a certain disease varies greatly. Right?
When you or someone hears that you have cancer, you will act in a certain way, which can be very different than when you hear someone has dementia, or you have dementia.
We act that way because of our perceived understanding of either one or both of the diseases. Our lack of understanding of either disease causes us to react differently. This is where the next area “Behavior Competence” comes into play.
“Behavioral Competence”

The last circle is the Behavioral Competence which includes language, physical function, physical health, activities, cognitive status, behavioral symptoms and balancing safety and autonomy.
That is a lot right. This circle on the left at 9 o’clock, is where executive function as well as physical function live.
This is also where physical health exists, as well as the amount of time you spend in activities that effect our cognitive status. It is about our behavioral systems and about balancing safety and autonomy.
When you think about it, this behavioral part is so critical, yet clearly not enough time is spent on it. As we move to the middle, then we can start thinking about how these things interact together
“Quality of Life, Sense of Personhood”
We can see how incorrectly perceived ideas about dementia can affect not only our mental health, but our physical health as well. Dementia can change how people react in terms of how people perceive our behavioral competence.

There are certainly many things that change in a person with dementia, but lack of understanding can dramatically affect how you take care of someone with dementia in terms of their physical environment.
Misunderstand it and you will do actual damage to the person, and this is where some real frustration and anger come from. I know it may not be intentional, but it happens.
Too many people are put in the wrong environment for a person with dementia because the caregiver is using a wrong perceived understanding. I hope you can you see how the wrong answer may have very wrong results.
If you can’t take care of a person, or you don’t think they can take care of themselves, then this might be where financial strain can become an issue. This also might become an issue that can affect both behavioral and perceived value of life. All these things interact in terms of the quality of life.
Dementia is not Aging[2]

The link above is to the NIH article on “Memory, Forgetfulness, and Aging: What’s Normal and What’s Not?”
Here what the NIH says under dementia and aging:
Dementia and Aging
“Dementia[3] is not a normal part of aging. It includes the loss of cognitive functioning — thinking, remembering, learning, and reasoning — and behavioral abilities to the extent that it interferes with a person’s quality of life and activities. Memory loss, though common, is not the only sign of dementia. People with dementia may also have problems with language skills, visual perception, or paying attention. Some people have personality changes.”
This is why it is important to level set people when they start talking about dementia, just like when someone says I have cancer. You need to know what kind. Just because you’re getting old and you’re forgetting things doesn’t mean you have dementia. All our brains like, our bodies deteriorate at different paces and that deterioration can cause lapses in memory and forgetfulness, but … actually feeling good about ourselves and doing routine daily activities can continue.
Dementia is different. Dementia is about cognitive thinking it’s about the ability to translate what we hear and or see into understanding cognitive information that is way different than just forgetting things.
Next, dementia is a broad label for lots of different things, it covers:

- Alzheimer’s
- Vascular dementia
- Lewy body dementia
- Parkinson’s
- Frontotemporal
- Creutzfeldt-Jakob
- Wernicke-Korsakoff
- Mixed dementia
- Normal pressure hydrocephalus
- Huntington’s disease
there are other causes or mixed causes
There are all sorts of different reasons that the brain is having problems with processing. Those differences make a big difference in how we act and how people need to care for people with those particular types of dementia.
So, when you have a loved one, or if you are the one with dementia and you’re trying to understand how do I get the best life possible while still having dementia, the answer is to understand how to create the right balance in life.
If we can achieve the “right” balance of life, we will significantly enhance psychological well-being, which we need to feel good about ourselves. We need to have purpose. We need to have a perceive value of life and a balance with physiological well-being.
Although they are tightly connected, obviously they are not the same. We need to address behavioral competence as we age. Obviously, our needs change as we get older.
Things change when you have dementia, too. The sooner you adjust to those changes or implement coping mechanisms or workarounds, the easier it will be for you to deal with the coming changes.
I have emphasize this over and over in my website Wanderinglite.com and DementiaTalks.net It is strategically important.
Get Ahead of Upcoming Changes
When you build coping [4]mechanisms and workarounds for things you help to address your weaknesses early, even before they become a problem. Then when they do become a real problem, they will not affect you as negatively as they could and your perceived value about yourself will not diminish.
Perceived negative value of yourself and of life starts by feeling that you can’t do things. Then that moves into diminishing psychological well-being. When our psychological well-being is threatened, we get depressed, and oh what a terrible tailspin this can be. This is Robin Williams Story and the genesis of “Robin’s Wish”.[5] So others will not suffer like Robin.
All these things are connected, all are about the quality of life. Developing this understanding of things that we can do early in our diagnosis and making changes are important. This is also why, getting an early diagnosis and of course not getting wrapped up about the stigma of dementia, means everything.
Helping other people understand what dementia really is, is so important because getting the right help in the right time will allow them to have a fruitful and healthy life, a “Good Life”.
Last, in case I forget, there are medications that work at the early stages of dementia and Alzheimer’s. But far too often stigmas get in the way. Early diagnosis means you can put coping mechanisms in place that help over the long run. Even simple thing like;

- making lists
- figuring out what interest brings you joy and purpose and forget the rest
- listening to music
- cooking
- changing you TV habits
- spending time with friend
And for me opening my heart and soul to God and whatever plans he has for me was everything.
I’m sure this Blog / Podcast, like the students that I have shared this information with before, will create lots of questions. Please go to WanderingLite.com and there you can post your questions, or you can connect with me and Wandering Lite on Facebook.
I will do my best to either to give you answers or connect you with somebody who has the answers.
I hope this helps. Sharing this message is the calling God gave me. He gave me the talents I have accumulated over my life, and now he calls me to use them to reach out and share, and I will do it as long as God and my health allow me.
Please share this message and my website… there are so many lost in unanswered questions.
Resources: Sixty and Me[6]
[1] Good Lives Model – https://www.sciencedirect.com/
[2] Memory, Forgetfulness, and Aging: What’s Normal and What’s Not? – NIH- National Institute on Aging – www.nia.nih.gov
[3] What Is Dementia? Symptoms, Types, and Diagnosis – NIH- National Institute on Aging – www.nia.nih.gov
[4] Healthy Coping: 24 Mechanisms & Skills For Positive Coping – positivepsychology.com
[5] https://www.robinswishfilm.com/
[6] https://sixtyandme.com/


No Comments